Padma’s mind was racing. Her doctor just told her she had leukemia. Padma (a fictitious name for this story) had never heard of leukemia. She was worried. “How long will I live? Will the treatments give me side effects? What will happen to my family? My husband? My two-year-old? We’re in the middle of the coronavirus. How will that affect my medical care?”
Indian Americans who are diagnosed with leukemia and other blood cancers face many challenges. Finding a stem cell match and, then, receiving a transplant is one of the only treatments to extend or save these patients’ lives.
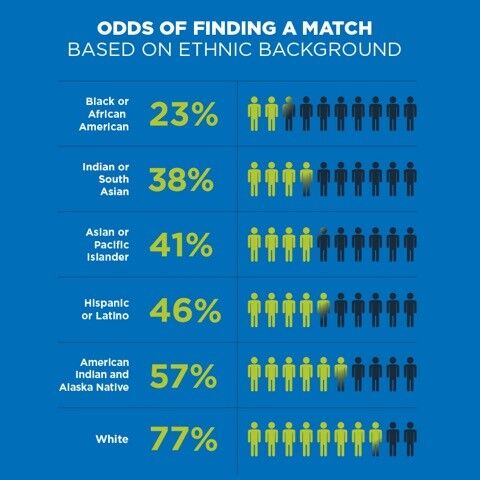
Indian Americans, however, are severely under-represented as stem cell donors. Seventy percent of the time, a stranger of your same ethnic background will be your stem cell match. Proportionally, there are more whites than Asians/Pacific Islanders on the Be The Match® national registry.
“What’s the solution?” asks Carol Gillespie, executive director of the Asian American Donor Program, a nonprofit in Alameda, California. “It’s to encourage more Indians, people of color and people who are of mixed racial/ethnic heritage to register as potential stem cell donors.”
Registering takes about five minutes. You complete the online registration and a swab kit is mailed to you. When you receive the kit, swab the inside of your cheek and pop the kit in the mail. Postage is pre-paid. You don’t have to leave your home and the testing is free.
Indian/South Asian donors only make up one percent of the national donor registry, leaving patients like Padma with only a 38% chance of finding a perfect stem cell match. Those who are on the registry are ready to save the life of any patient anywhere in the world who is in need of a stem cell match and transplant.
AADP is working with Veer, a 3-year-old Indian boy who lives in Canada, and Layla, a 2-year-old Indian girl who lives in the United Kingdom. Both urgently need to find a stem cell donor to extend their lives.
COVID-19 Adds Complications
The coronavirus has had a dismal impact upon patients diagnosed with blood cancers. Patients are afraid that a life-saving donor will not be found in time. They are scared that if a matching donor is found, that person, because of COVID-19, will not want to go to a clinic to have their stem cells collected.
“With the coronavirus pandemic and the need for six-foot distancing, we have cancelled our in-person community registration events,” Gillespie said. “So, our community education and awareness efforts, which generate new donors, are suffering and blood cancer patients are worried.”
Vivek Kumar
For Vivek Kumar, who is originally from Mumbai, within a few years of his registering as a donor, he was told he was a stem cell match for a woman in India.
“Of all the people in the world, I was her match,” Vivek says. “We were genetic cousins of sorts. I was committed to giving her my stem cells.”
“Don’t hesitate to register,” he says. “All it takes is a simple swab of the inside of your cheek. Why wouldn’t you want someone with a blood cancer to live several more years?”
Vivek poses the question: What if this was someone in your family and a potential donor was hesitating to register?
“Donating was a few days of inconvenience,” he said. “How can you compare that with the impact of saving a life? We can each do our own part.”
Dinesh Chandrasekhar
Dinesh and his wife registered with AADP as potential stem cell donors at a registration event at a Hindu temple.
He was notified that he was a stem cell match for a patient. On having his vitals checked, Dinesh discovered that his blood pressure was abnormally high. So, the procedure was called off. “I was never more disappointed in my life,” he says. “It was a huge shock that I could not donate.”
After an appointment with his primary doctor, Dinesh started medication and his blood pressure normalized.
Again, Dinesh was told he was a match for a patient. His vitals were good and, in April 2015, he donated his peripheral blood stem cells. It ended up that Dinesh donated for the same patient about whom he was initially contacted. “We are both the same age. It was like destiny,” Dinesh says.
Donating took about four hours. At the hospital, Dinesh’s blood was removed from his arm and cycled through a machine that separates the stem cells from the other blood cells. His stem cells were kept in a separate bag, while the rest of his blood was returned to him. During this time, Dinesh watched TV shows.
“Giving your stem cells is not like you are donating a part of your body (kidney, liver, etc.),” Dinesh says.
Before going to a clinic or hospital, donors are given shots that stimulate white blood cell production. “This production moves blood stem cells from the marrow into the bloodstream so that the stem cells can be collected from the donor,” says Gillespie. “So, you are missing nothing.”
“The next morning I felt normal and went back to work. Now that I have done this, I would do it again,” Dinesh says.
Six months later, Dinesh was told that his recipient was doing well and back to their normal life.
“As human beings, we are here to help each other,” Dinesh says. “I encourage everyone to register as a stem cell donor and be committed to donating your stem cells when you are called.”
Ethnicity Matters
Ethnicity is key when looking for a stem cell match. Matching is based on your human leukocyte antigen (HLA) tissue type. Your HLA is part of what makes you ‘you’ – your individual genetic characteristics. So, HLA matches are closely based upon a patient’s ethnicity.
The lack of ethnic diversity on the Be The Match® national registry makes it difficult for patients to find a stem cell match.
Join the registry by texting AADP to 61474, or visit AADP.
Original Content: www.indiawest.com




Leave a Reply